
When a patient’s condition deteriorates in the ward, it can be a stressful and challenging situation for both healthcare professionals and the patient’s family. Prompt and effective action is essential to ensure the best possible outcome. When I first started my rotation, it was a horrible situation for me and I always wanted to not get into any such situation without the assistance of my senior. But with time, I got confidence and I was the one who taught others about such challenging situations. Here’s a comprehensive guide on how to manage a deteriorating patient in the ward from me to you:
1. Initial Assessment and Updating Family
Whenever the family member rush to you to see their patient, remember:
- Stay Calm: Keep calm and focused. Leave your work and go to the patient and in doing so remember the disease of the patient and what complications could have had occured to the patient.
- Assessment: Assess the patient’s ABCDEs (Airway, Breathing, Circulation, Disability, Exposure). Also the assessment includes the following
- Temperature
- Pulse rate
- Respirations
- oxygen sats
- glucose levels
- Blood pressure
- capillary refill time (CRT)
- level of consciousness
- Call for Help: If the patient is critically ill, call for assistance from a senior colleague or the Rapid Response Team. You can call a code too.
- Assess Vital Signs: Check the patient’s vital signs, including heart rate, blood pressure, respiratory rate, oxygen saturation, and temperature.
- Neurological Assessment: Perform a brief neurological assessment, including level of consciousness, pupil size, and response to stimuli.
Updating Family:
- Designated Spokesperson: Designate one healthcare professional to communicate with the family.
- Provide Reassurance: Reassure the family that the patient is receiving the best possible care.
- Explain the Situation: Use clear, jargon-free language to explain the patient’s condition and the actions being taken.
- Encourage Questions: Encourage the family to ask questions and express their concerns.
- Regular Updates: Provide regular updates on the patient’s condition and any changes in treatment.
2. Monitoring and Observations
Continuous Monitoring:
- Frequent Observations: Increase the frequency of observations according to the patient’s condition.
- Continuous Cardiorespiratory Monitoring: Consider continuous cardiac and oxygen saturation monitoring for high-risk patients.
- Neurological Monitoring: Monitor the patient’s level of consciousness and neurological status regularly.
Clinical Observations:
- Respiratory Rate: Monitor the patient’s respiratory rate and effort.
- Oxygen Saturation: Check oxygen saturation regularly and administer oxygen therapy as needed.
- Blood Pressure: Monitor blood pressure closely, especially in hypotensive patients.
- Fluid Balance: Assess fluid balance and urine output regularly.
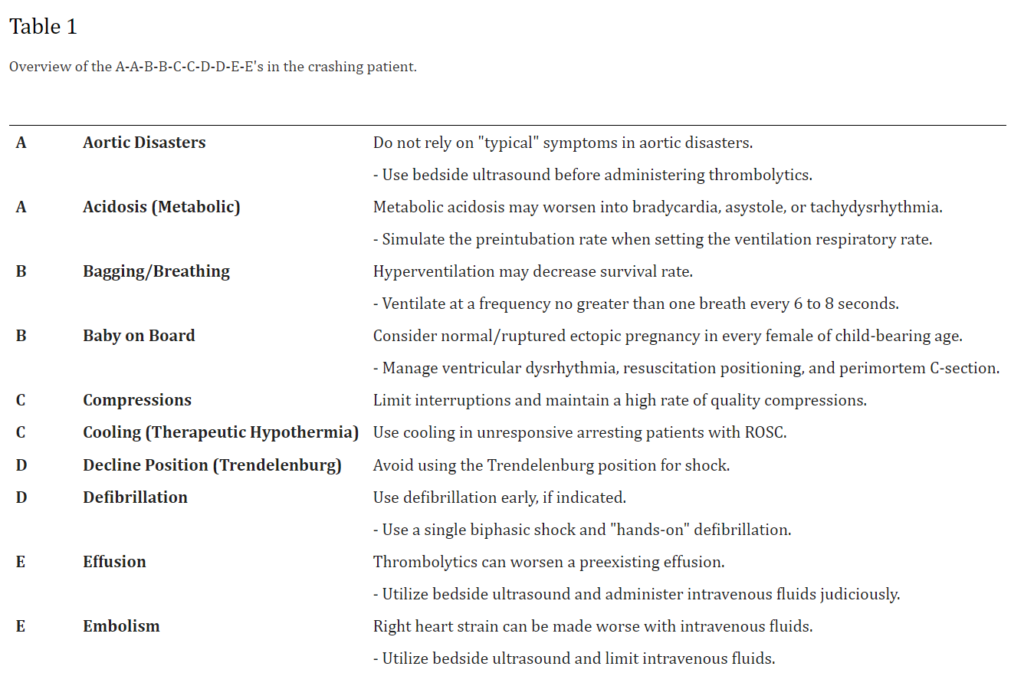
Expending resources and time in pursuit of a misdiagnosis will further harm an already unstable patient. Here I will quote the NCBI Article: To improve physician response and competence in crisis, we present an easily remembered mnemonic, the A-A-B-B-C-C-D-D-E-E’s in the crashing patient, Read here; https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3248865/
3. Treatment and Interventions
Position the patient
- Depending on how the patient presents, will depend on the position that you put your patient in. You will generally be guided by your patient’s vital signs and symptoms.
Some of the common positions include:
- Patients who are unconscious but breathing normally should be placed in the recovery position (as long as no spinal injury is suspected).
- If the patient is hypotensive, they should be laid flat with their legs elevated.
- If the patient appears breathless they should be moved into a fowler’s or semi-fowler’s position.
- If the patient has suspected acute coronary syndrome, they should be placed into a semi-upright position.
Oxygen Therapy:
If the patient is getting short of breath and has no heart condition and ECG also came right, then it is the lungs;
- Administer Oxygen: Administer oxygen therapy to maintain oxygen saturation within the target range.
- Consider Non-Invasive Ventilation: Consider non-invasive ventilation for patients with respiratory distress.
Fluid Resuscitation:
- Assess Fluid Status: Assess the patient’s fluid status and consider fluid resuscitation if indicated.
- Intravenous Access: Ensure adequate intravenous access for fluid administration.
Medication Management:
- Administer Medications: Administer medications as prescribed, including antibiotics, vasopressors, and analgesics.
- Monitor Response: Monitor the patient’s response to medications and adjust treatment as needed.
If nothing goes right and the patient stops breathing with no pulse, start CPR and ask for assistance. Otherwise, you just have to make a Death certificate. But Remember, Cardiopulmonary resuscitation should not be the sole focus of your care plan.
4. Communication and Documentation
Communication:
- Effective Communication: Maintain open and honest communication with the patient, family, and multidisciplinary team.
- Document Everything: Document all assessments, interventions, and communications in the patient’s medical record.
Review and Reassessment:
- Regular Review: Regularly review the patient’s condition and response to treatment.
- Reassessments: Reassess the patient’s ABCDEs and vital signs frequently.
Debriefing:
- After the Event: Arrange a debriefing session with the healthcare team after the patient’s condition has stabilized.
- Discuss the Event: Discuss what went well and identify areas for improvement.

Conclusion
Managing a deteriorating patient in the ward requires prompt assessment, effective communication, and coordinated action. By following the steps outlined in this guide, healthcare professionals can ensure that patients receive the best possible care during times of crisis. Remember, early recognition and intervention can significantly improve patient outcomes.


